Alimentary System
Oral Mucosa - Necrosis
Narrative
Brown HR, Hardisty JF. 1990. Oral cavity, esophagus and stomach. In: Pathology of the Fischer Rat (Boorman GA, Montgomery CA, MacKenzie WF, eds). Academic Press, San Diego, CA, 9-30.
Abstract: https://www.ncbi.nlm.nih.gov/nlmcatalog/9002563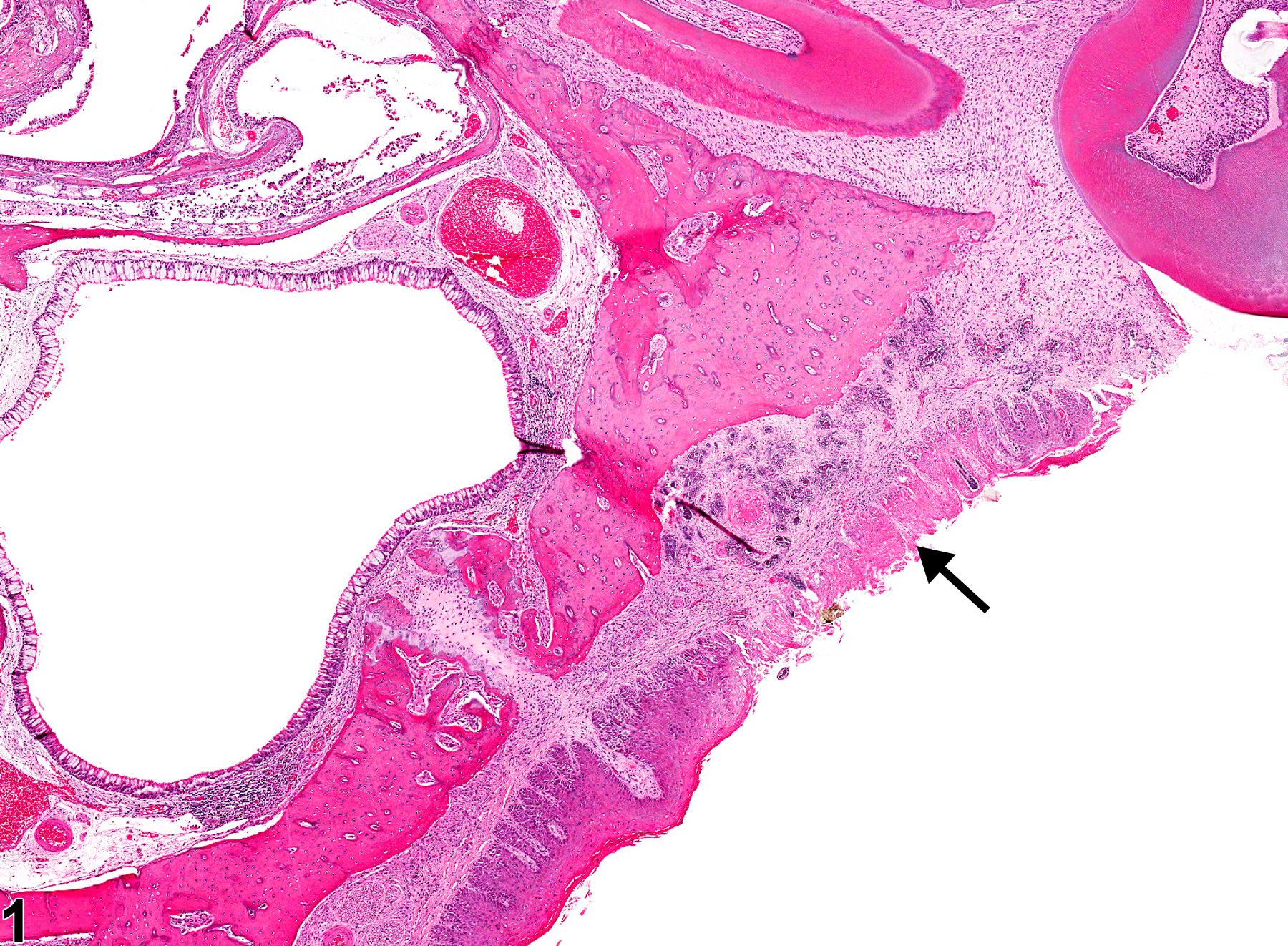
Oral mucosa - Necrosis in a male F344/N rat from a subchronic study. There is necrosis of the epithelium on the hard palate (arrow).