Cardiovascular System
Heart - Inflammation
Narrative
Valvular inflammation commonly refers to an inflammatory lesion of the heart valves. The diagnostic features include the presence of vegetative plaques composed of mixed inflammatory cells including neutrophils in a matrix of fibrin that may also contain colonies of bacteria. Hemorrhage may be present in the underlying valvular stroma, and reactive hyperplasia may be present in the adjacent endothelium or underlying stromal cells. Valvular endocarditis may be an incidental finding. Lesions may be consistent with sepsis, and other organs should be examined for evidence of septicemia.
In NTP studies, there are five standard categories of inflammation: acute, suppurative, chronic, chronic-active, and granulomatous. In acute inflammation, the predominant infiltrating cell is the neutrophil, though fewer macrophages and lymphocytes may also be present (Figure 1). There may also be evidence of edema or hyperemia. The neutrophil is also the predominant infiltrating cell type in suppurative inflammation; however, in suppurative inflammation the neutrophils are aggregated, and many of them are degenerate (suppurative exudate). Cell debris, from both the resident cell populations and infiltrating leukocytes; proteinaceous fluid containing fibrin; fewer macrophages and occasional lymphocytes or plasma cells; and, possibly, an infectious agent may also be present within the exudate. Grossly, these lesions would be characterized by the presence of pus (Figure 2 and Figure 3). In the tissue surrounding the exudate, there may be fibroblasts, fibrous connective tissue, and mixed inflammatory cells, depending on the chronicity of the lesions. Lymphocytes predominate in chronic inflammation (Figure 4, Figure 5, and Figure 6). Lymphocytes also predominate in chronic-active inflammation, but there are also a significant number of neutrophils (Figure 7 and Figure 8). Both suppurative and chronic-active inflammation may contain macrophages. Granulomatous inflammation is another form of chronic inflammation, but this diagnosis requires the presence of a significant number of aggregated, large, activated macrophages, epithelioid macrophages, or multinucleated giant cells. Inflammation is differentiated from cellular infiltrates by the presence of other changes, such as edema, hemorrhage, degeneration, necrosis, or other evidence of tissue damage.
Wachtman LM, Browning MD, Bedja D, Pin S, Gabrielson KL. 2006. Validation of the use of long-term indwelling jugular catheters in a rat model of cardiotoxicity. J Am Assoc Lab Anim Sci 45(5):55-64.
Abstract: https://www.ncbi.nlm.nih.gov/pubmed/16995648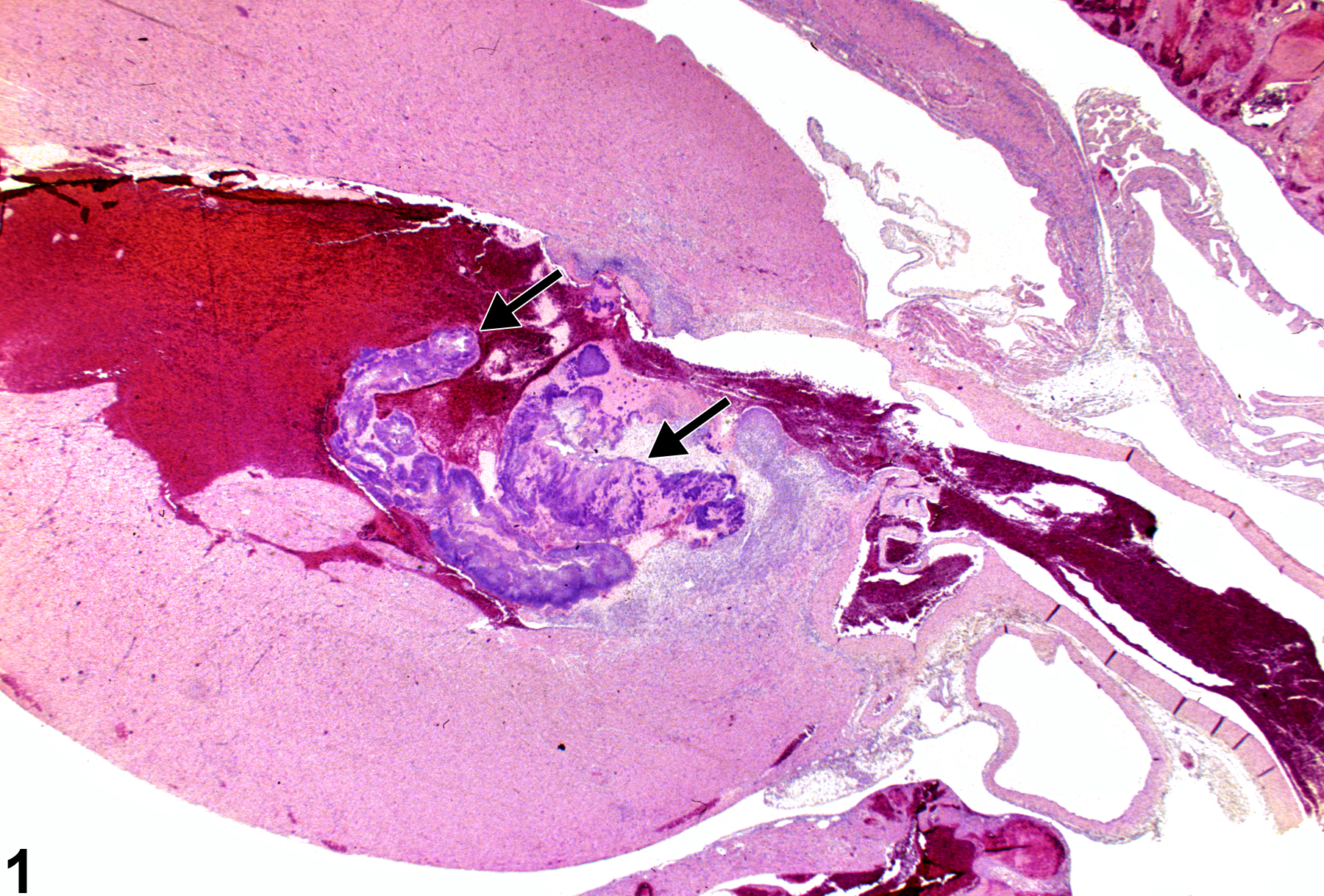
Heart, Valve - Inflammation, Acute in a female F344/N rat from a chronic study. Neutrophils (arrows) are present within a valve.