Alimentary System
Tongue - Necrosis
Narrative
Comment:
Necrosis can occur secondary to trauma, infection, vasculitis, or thrombosis or as a direct effect of a test agent (particularly epithelial necrosis). Necrosis is differentiated from ulcer in that an ulcer is an area of loss of squamous epithelium that extends through the basement membrane, exposing the underlying lamina propria. In necrosis, the necrotic epithelium remains attached to the basement membrane. Necrosis may involve the full thickness of the tongue (Figure 1, Figure 2, Figure 3, and Figure 4), particularly when the etiology is vascular. In addition to muscle necrosis (Figure 2, Figure 4, Figure 5, and Figure 6, arrows), the overlying squamous epithelium of the tongue can also be necrotic (Figure 2 and Figure 3, arrows), depending on the location and extent of necrosis. Inflammation often accompanies the necrosis, and the type of inflammation present depends on the chronicity and the etiology. Lesions are not common in the muscle of the tongue in NTP studies.
Recommendations:
Necrosis should be diagnosed and given a severity grade. If the necrosis involves muscle or multiple tissues in the tongue, then it is diagnosed as "tongue - necrosis." However, if the necrosis is limited to the epithelium of the tongue, the diagnosis should be "tongue, epithelium - necrosis." Secondary lesions, such as inflammation or hemorrhage, generally should not be diagnosed separately unless they are prominent components of the lesion. If the necrotic lesion is consistent with an infarct, it should be diagnosed as "necrosis," but the pathology narrative should state the lesion is consistent with an infarct.
References:
Westwood FR, Jones DV, Aldridge A. 1996. The synovial membrane, liver, and tongue: Target organs for a ricin A-chain immunotoxin (ZD0490). Toxicol Pathol 24:477-483.
Abstract: https://www.ncbi.nlm.nih.gov/pubmed/8864189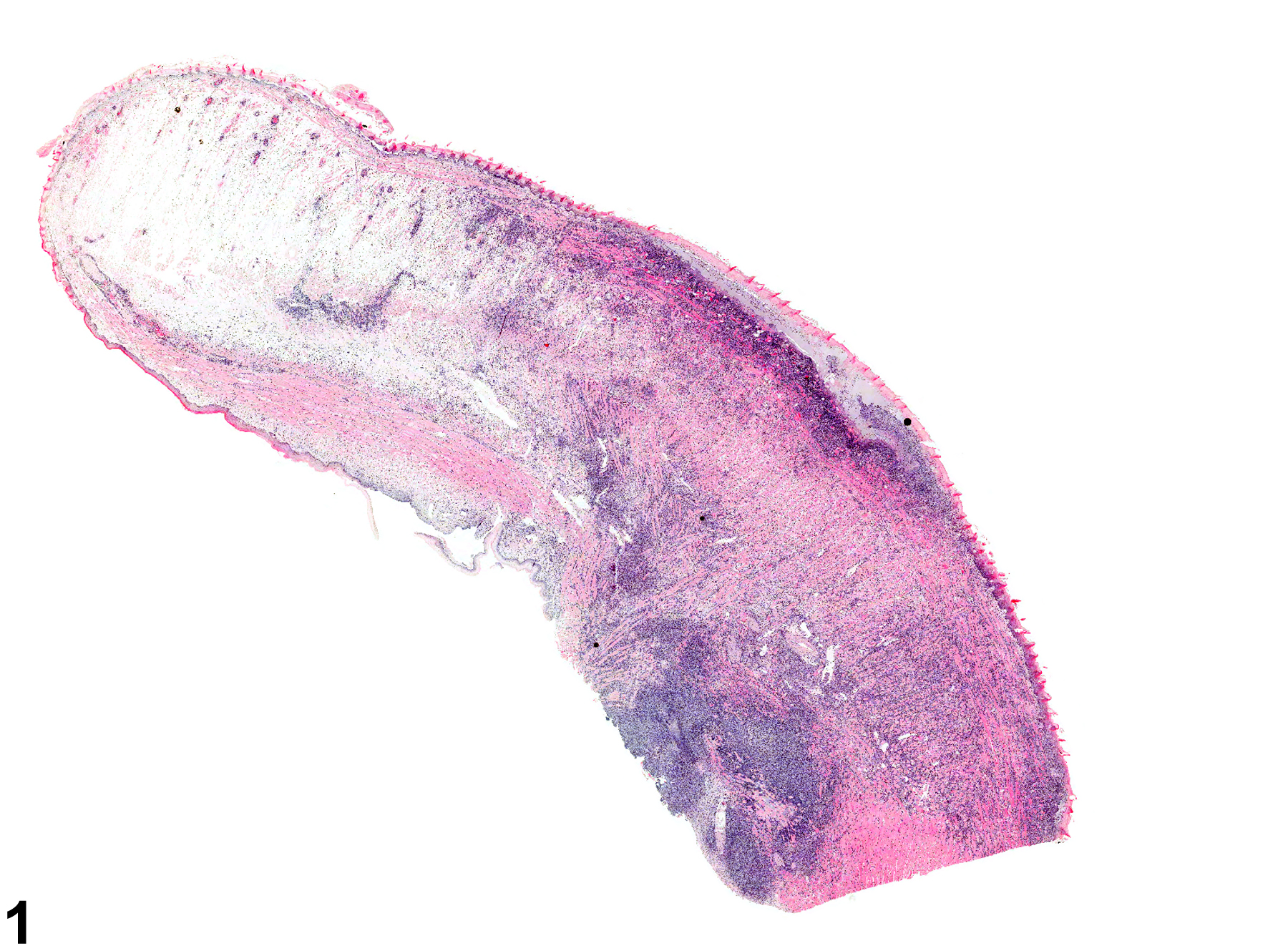
Tongue - Necrosis in a male Swiss CD-1 mouse from a chronic study. There is widespread necrosis of the tip of the tongue.