Alimentary System
Oral Mucosa - Ulcer
Narrative
Klein-Szanto AJP, Conti CJ, Aldaz CM. 1990. Skin and oral mucosa. In: Handbook of Toxicologic Pathology (Haschek WM, Rousseaux CG, eds). Academic Press, San Diego, CA, 85-119.
Abstract: http://www.sciencedirect.com/science/book/9780123302151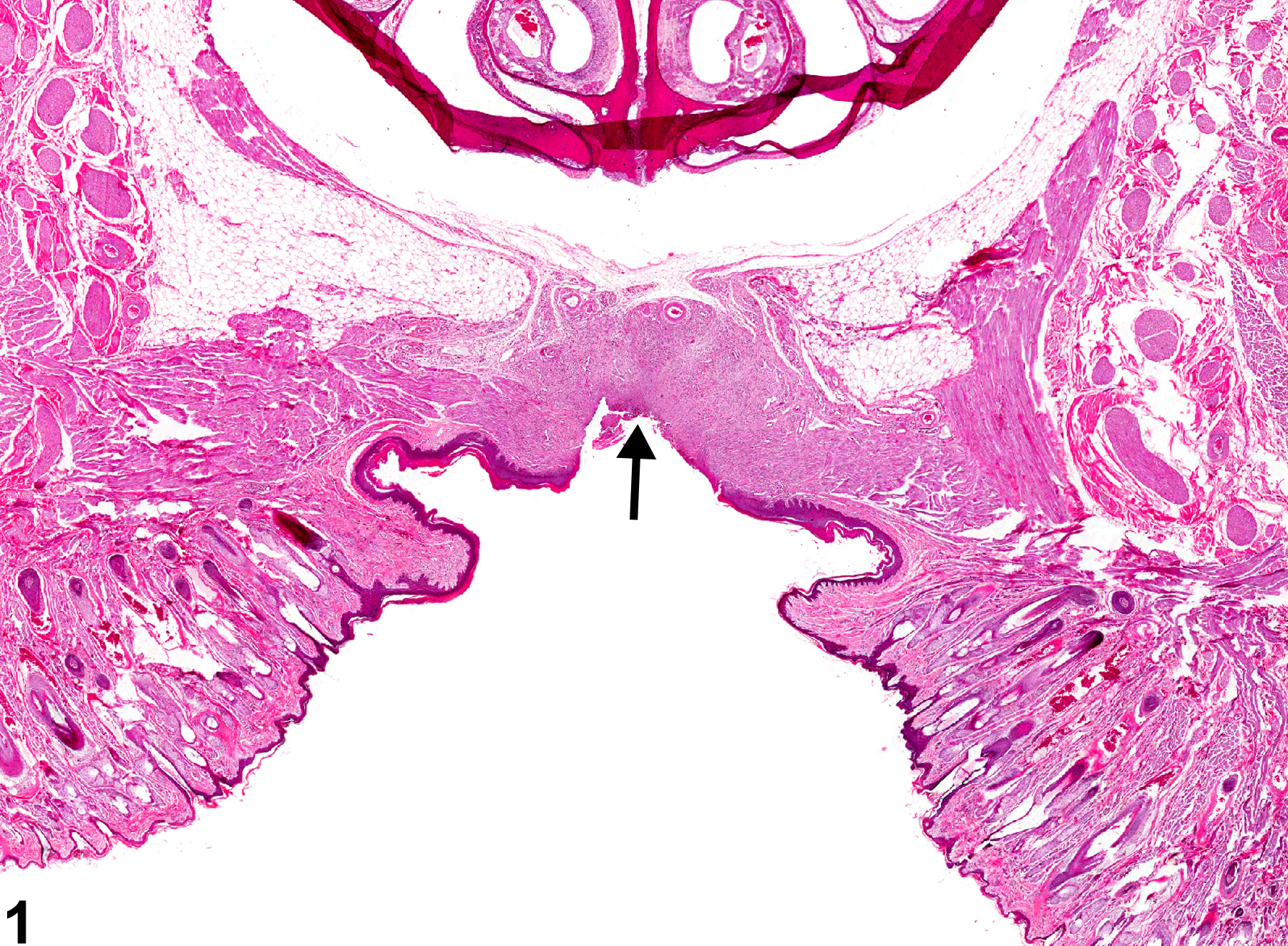
Oral mucosa - Ulcer in a female F344/N rat from a chronic study. A portion of the hard palate mucosa is absent (arrow), exposing the underlying connective tissue.