Alimentary System
Stomach, Glandular Stomach - Inflammation
Narrative
Inflammation can be diagnosed as acute, suppurative, chronic, chronic active, or granulomatous. In acute inflammation, the predominant infiltrating cell is the neutrophil, though fewer macrophages and lymphocytes may also be present. There may also be evidence of edema or hyperemia. The neutrophil is also the predominant infiltrating cell type in suppurative inflammation, but the neutrophils are aggregated, and many of them are degenerate (suppurative exudate). The exudate may also contain cell debris, both from the resident cell populations and from infiltrating leukocytes; proteinaceous fluid containing fibrin; fewer macrophages; occasional lymphocytes or plasma cells; and, possibly, an infectious agent. Grossly, these lesions would be characterized by the presence of pus. In the tissue surrounding the exudate, there may be fibroblasts, fibrous connective tissue, and mixed inflammatory cells, depending on the chronicity of the lesion. Lymphocytes predominate in chronic inflammation. Lymphocytes also predominate in chronic active inflammation, but there are also a significant number of neutrophils. Both lesions may contain macrophages. Granulomatous inflammation is another form of chronic inflammation, but this diagnosis requires the presence of a significant number of aggregated, large, activated macrophages, epithelioid macrophages, or multinucleated giant cells.
Eosinophilic inflammation (Figure 3 and Figure 4) is not one of the five main types of inflammation ordinarily diagnosed by the NTP but may be diagnosed if the inflammatory cells are primarily eosinophils. The pathologist may deviate from the 5 main inflammation diagnoses as long as the reason for the deviation is discussed in the narrative.
Leininger JR, Jokinen MP, Dangler CA, Whiteley LO. 1999. Oral cavity, esophagus, and stomach. In: Pathology of the Mouse (Maronpot RR, ed). Cache River Press, St Louis, MO, 29-48.
Abstract: http://www.cacheriverpress.com/books/pathmouse.htm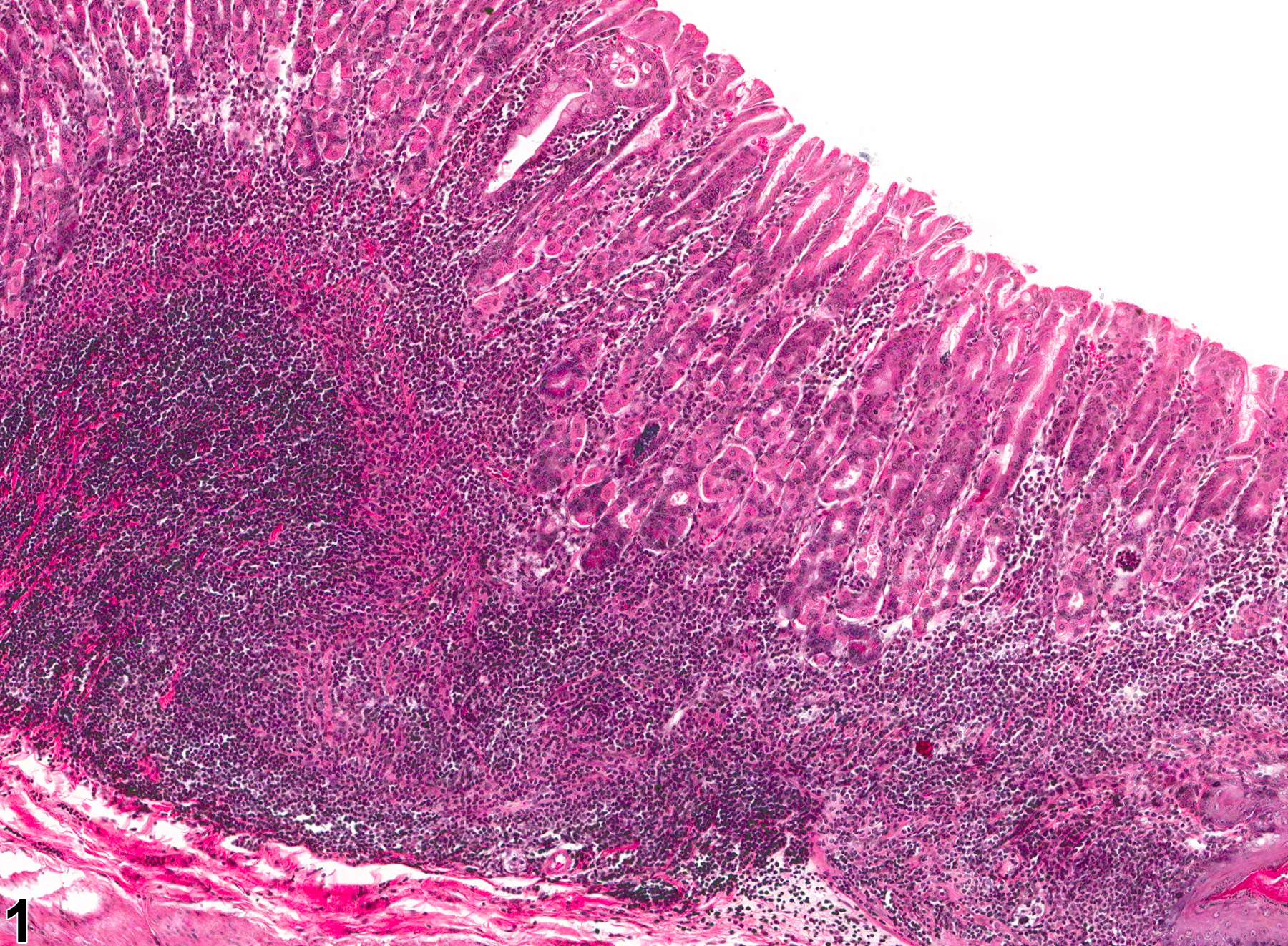
Stomach, Glandular stomach - Inflammation, Chronic in a male B6C3F1 mouse from a chronic study. Lymphocytes (primarily) are present within the submucosa and lamina propria.